Lithium remains a cornerstone in the management of bipolar disorder and other affective illnesses, yet its adverse effects often challenge long-term adherence. Among its wide range of side effects, erectile dysfunction (ED) and sexual disturbances stand out for their profound impact on quality of life. For a patient struggling with mood instability, the added burden of impaired sexual health can create a cycle of non-compliance, worsening psychiatric symptoms, and overall functional decline. This article explores the neurobiology, epidemiology, and mechanistic underpinnings of lithium-associated erectile dysfunction, while also examining therapeutic strategies—including the potential role of sildenafil and other phosphodiesterase type 5 (PDE5) inhibitors.
Lithium: A Double-Edged Sword in Psychiatry
Lithium, first introduced to psychiatry in 1949, has saved countless lives through its ability to reduce mania, stabilize mood, and lower suicide risk. It exerts complex molecular effects: inhibition of glycogen synthase kinase-3β, interference with inositol monophosphate pathways, modulation of circadian rhythms, and alterations in neurotransmitter signaling. These effects underpin its therapeutic benefits but also contribute to its side-effect profile.
Patients treated with lithium frequently report tremor, renal dysfunction, thyroid abnormalities, and gastrointestinal disturbances. Less commonly discussed but equally disruptive are sexual side effects. Sexual health is not merely a matter of intimacy—it is a determinant of compliance and self-esteem. Clinical observations suggest that nearly one-third of men treated with lithium report diminished libido, difficulty maintaining erections, or decreased satisfaction during intercourse.
The paradox of lithium is clear: it saves lives in one domain while silently eroding quality of life in another. Understanding the biological foundations of this problem is the first step toward solutions.
Neurophysiology of Penile Erection: A Delicate Balance
Erectile function is orchestrated by a symphony of central and peripheral mechanisms. Neural circuits spanning the hypothalamus, hippocampus, spinal cord, and pelvic plexuses converge on the penis, where cavernosal smooth muscle responds to neurotransmitter release. Dopaminergic signaling from the medial preoptic area, oxytocinergic activity in the paraventricular nucleus, and nitric oxide release from cavernosal nerves all promote erection.
The nitric oxide (NO)–cGMP pathway is pivotal. Upon sexual stimulation, neuronal nitric oxide synthase (nNOS) and endothelial nitric oxide synthase (eNOS) generate NO, which activates guanylyl cyclase, increasing cGMP levels and inducing smooth muscle relaxation. This cascade enables blood inflow into the corpora cavernosa, trapping venous outflow, and producing penile rigidity.
Disruption at any level—whether central neurotransmission, endothelial health, or smooth muscle responsiveness—can lead to erectile failure. Unfortunately, lithium’s pharmacologic actions intersect with multiple nodes in this pathway, explaining its impact on sexual function.
Clinical Evidence of Lithium-Associated Sexual Dysfunction
Reports of lithium’s sexual side effects date back to the 1970s. In early observational studies, men treated with lithium frequently described reduced libido, impaired erectile capacity, and premature detumescence. Subsequent clinical surveys confirmed these findings:
- Up to 30–35% of male patients on lithium report significant erectile or sexual dysfunction.
- Dysfunction is not strictly dose-dependent and may occur at both therapeutic and subtherapeutic serum concentrations.
- Combination therapy with benzodiazepines or anticonvulsants appears to exacerbate sexual side effects compared to lithium monotherapy.
- Cross-sectional studies indicate that lithium-treated patients engage in fewer sexual fantasies, less frequent intercourse, and derive less satisfaction from sexual activity compared to matched controls.
Importantly, sexual side effects strongly correlate with poor adherence. In one study, men reporting lithium-induced dysfunction were more likely to miss doses or discontinue therapy altogether. This raises not only a clinical problem but a public health concern, as non-compliance increases relapse and suicide risk.
Mechanistic Insights: How Lithium Disrupts Sexual Function
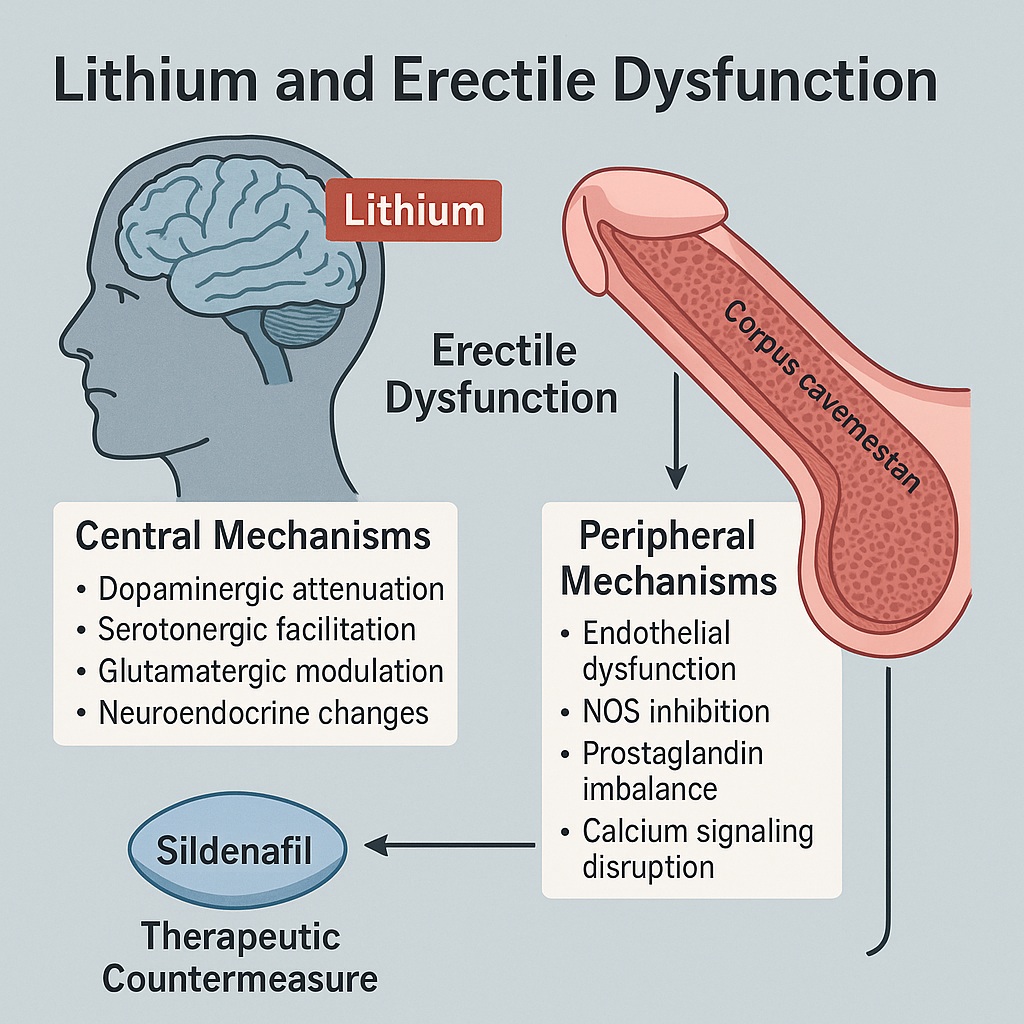
Lithium interferes with sexual function via central and peripheral pathways.
Central Mechanisms
- Dopaminergic attenuation: Lithium reduces dopamine release in key brain regions and impairs receptor signaling. Given dopamine’s facilitatory role in erection, this leads to diminished sexual drive and arousal.
- Serotonergic facilitation: Lithium enhances serotonin transmission, particularly at postsynaptic 5-HT receptors, which exert inhibitory effects on sexual reflexes.
- Glutamatergic modulation: By dampening NMDA receptor activity, lithium may blunt excitatory neurotransmission needed for erectile initiation.
- Neuroendocrine changes: Lithium alters hypothalamic-pituitary-adrenal (HPA) axis function and may reduce testosterone levels, compounding its central inhibitory actions.
Peripheral Mechanisms
- Endothelial dysfunction: Chronic lithium exposure impairs acetylcholine-induced, endothelium-mediated cavernosal relaxation, largely by reducing NO bioavailability.
- NOS inhibition: Lithium decreases both nNOS and eNOS activity, leading to reduced NO synthesis in penile tissue.
- Prostaglandin imbalance: Lithium disrupts cyclooxygenase pathways, tipping the balance toward vasoconstrictors (e.g., PGF2α) rather than vasodilators (e.g., PGE1, PGE2).
- Calcium signaling disruption: By interfering with inositol phosphate and intracellular calcium dynamics, lithium blunts endothelial responses critical for cavernosal smooth muscle relaxation.
Collectively, these pathways illustrate lithium’s multipronged attack on sexual health.
Therapeutic Strategies: Can the Damage Be Mitigated?
Given lithium’s irreplaceable psychiatric benefits, discontinuation is rarely advisable. Instead, clinicians must seek strategies to manage its sexual side effects.
Aspirin and Cyclooxygenase Inhibitors
A randomized trial found that aspirin significantly improved erectile function in men with lithium-induced ED, likely through modulation of prostaglandin pathways. This aligns with preclinical findings where indomethacin improved cavernosal relaxation in lithium-treated rats.
PDE5 Inhibitors
The most logical intervention remains the use of sildenafil and related PDE5 inhibitors. By augmenting the NO–cGMP pathway, these drugs counteract lithium’s suppression of endothelial and neuronal signaling. Clinical experience shows marked improvement in erectile quality among men on lithium when treated with sildenafil, making it the frontline adjunctive therapy.
L-Arginine Supplementation
Experimental studies suggest that L-arginine, a substrate for NO synthesis, restores endothelial function in lithium-exposed penile tissue. While not yet validated in clinical trials, it represents a low-risk intervention worth further study.
Hormonal Considerations
Where testosterone deficiency is present, replacement therapy may be appropriate. Lithium has been shown to reduce testosterone in some animal models, and correcting this deficit may restore libido and erectile capacity.
Lithium, Sexual Health, and the Psychiatric Patient: The Human Dimension
The challenge of lithium-induced ED is not merely biochemical—it is profoundly human. Patients already grappling with mood instability face an added layer of distress when sexual function declines. This can fracture relationships, erode confidence, and worsen psychiatric outcomes.
Clinicians must approach this issue proactively. Too often, sexual health remains unspoken in psychiatric consultations. Open dialogue, routine screening, and early intervention are critical. The ability to say to a patient, “Yes, lithium may cause these issues, but we have strategies—sildenafil, aspirin, supplementation—that can help,” may spell the difference between continued adherence and silent discontinuation.
Future Directions: Toward Integrated Care
Research must move toward:
- Large-scale clinical trials testing PDE5 inhibitors, aspirin, and L-arginine specifically in lithium-treated patients.
- Mechanistic studies clarifying how lithium alters NO synthase isoforms in penile and neural tissue.
- Development of mood stabilizers with lithium’s psychiatric efficacy but without its sexual toxicity.
For now, the integration of psychiatric and sexual medicine offers the best hope for patients. Urologists and psychiatrists must collaborate, recognizing that mental stability and sexual health are not mutually exclusive goals.
FAQ
1. Why does lithium cause erectile dysfunction?
Lithium interferes with both brain neurotransmitters and penile endothelial function, reducing dopamine and NO signaling while enhancing inhibitory serotonin activity. This dual effect disrupts both sexual desire and erection.
2. Can sildenafil help with lithium-induced erectile dysfunction?
Yes. Sildenafil and other PDE5 inhibitors improve erectile capacity by enhancing the NO–cGMP pathway, directly countering one of lithium’s main mechanisms of dysfunction.
3. Is lithium-induced ED permanent?
No. Sexual function often improves after dose adjustment, discontinuation, or the addition of therapies such as sildenafil. In most cases, the dysfunction is reversible.
4. Should patients stop lithium if they develop ED?
Not without medical supervision. Lithium remains vital for bipolar disorder management. Instead of discontinuing, patients should discuss adjunctive therapies—including PDE5 inhibitors, aspirin, or hormonal assessment—with their physician.